For peace of mind, remember to always pre-authorise your treatment
Pre-authorisation gives you an extra level of reassurance, so you can rest easy knowing your treatment will be covered under your plan, well before you make a claim.
Our team is here any time, day or night, to help guide you through the process and make sure you’re getting the right treatment for your needs. This includes a second opinion from international experts, so you are fully comfortable with your treatment plan before committing.

Seamless experience
Pre-authorisation allows us to settle claims directly with providers in our network, so you can focus on your immediate health needs without the hassle of handling payment further down the line.

Complete reassurance
By pre-authorising, you’ll be able to start your treatment knowing for certain that it’s covered. You can also ask for a second medical opinion to ensure you are pursuing the right course of care.
How do I pre-authorise my treatment?
If you’ve been advised to seek treatment, start the pre-authorisation process through MembersWorld, either online or in-app.
You can also do this via phone or email. Make sure you have your membership number to hand.
If you haven’t yet booked your treatment, use the Facility Finder to identify a provider within Bupa Global’s extensive network of two million providers.
What do I need to get started?
To begin pre-authorisation for your treatment:
- You’ll need to provide us with details of your symptoms, diagnosis, and procedure.
- If you’ve already booked your treatment, we’ll require information about when and where it will take place and the clinician who will oversee your treatment.
- We might ask for more information, like a medical report from your healthcare professional that details your condition, including your symptoms and how long you have been experiencing them, and the treatment path they’re recommending.
- If you have received tests already, for example an X-ray or blood tests, please ask for copies of the results from your healthcare professional as we may ask for them during pre-authorisation, so it can speed things up if you have them ready.
How do I settle my claim?
If you are treated by a provider in our network, pre-authorisation allows Bupa to directly settle with the provider. This way, you’ll also ensure treatment charges are covered, avoiding any shortfalls.
If your provider isn’t in our network, you should submit a claim through MembersWorld. If you pay then claim, we’ll also ask you for proof of payment along with any invoices.
We will only cover reasonable and customary costs for providers outside of our network. This means we cannot guarantee payment will be made in full for treatment received outside of our network, even if pre-authorised.
You can avoid any such claim shortfalls by choosing from Bupa Global’s extensive network of over two million providers. By opting for treatment with these approved providers, pre-authorisation ensures no payment from you at the point of treatment.
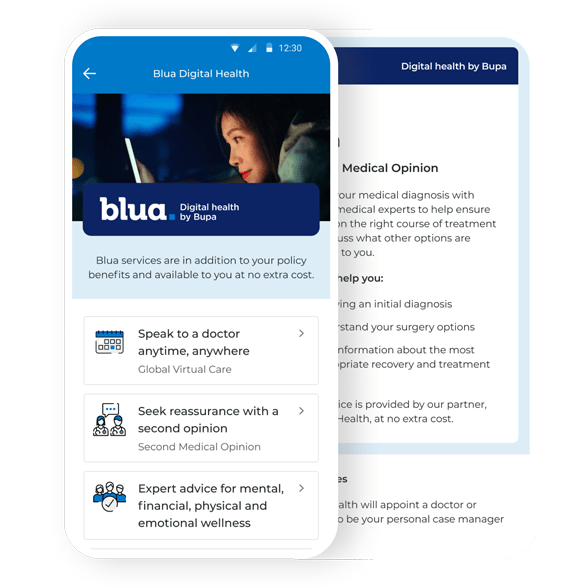
Manage your plan with MembersWorld
Did you know the quickest way for existing members to contact us is to send a direct message on MembersWorld? What’s more, you can also:
- View your policy document and access your membership card
- Pre-authorise treatment
- Submit, track and review a claim
- Prescriptions and referral letters sent directly to your phone, where local regulations allow.
Get started today by downloading the MembersWorld app or sign in to your account .